It’s time for research updates! BDSRA Foundation’s Head of Research & Medical Affairs Dr. Ineka Whiteman breaks down Batten disease clinical program updates, research news & opportunities, and resources in her monthly column, as seen in BDSRA’s monthly newsletter, The Illuminator.
Annual Family Conference 2024 – Science and Clinical Program Highlights
What a weekend!! I was absolutely blown away by the atmosphere, sense of community, robust discussions, and engagement of attendees this year. This is my third consecutive year attending the conference in person and I can honestly say, it feels bigger and better every year.
The conference kicked off with the main Research Session on Friday morning. Presentations covered Batten research advances “from lab bench to bedside,” including cell and animal models, biomarker discovery, and preclinical therapies. The session finished with the latest clinical trial updates and an open, lively Q&A session with academic and clinical researchers, and biotech company representatives. Day two kicked off with the popular 90-minute “Ask-A-Doc” session, where families could ask impromptu questions to a panel of six Centers of Excellence (CoE) and Affiliate Center directors. In the afternoon, more than 20 clinicians representing nine Centers came together for its second in-person Center of Excellence Working Party meeting to continue developing collaborative opportunities and network projects to advance clinical education, research, and best practices in Batten disease care.
Other science and clinical program highlights throughout the weekend included concurrent sessions on “Behavior, Cognition and Learning,” “Palliative Care: Debunking the Stigmas,” Case Management 101 and the “Ask Me Anything: Scientists Edition” with research scientists who were delighted to share a collection of laboratory gadgets and research tools for attendees to try out, and to answer a variety of curious questions on their laboratory research. Our sincerest thanks and appreciation to all speakers and panelists who willingly offered to contribute their time and expertise to this robust program. And my gratitude to Dr. Jon Cooper and Dr. David Pearce for their help in pulling together some of our best science, clinical, and SIBs sessions yet!
Some sessions mentioned here were recorded and are now available in the conference app.
A huge, heartfelt thanks to all our families who participated in the many onsite research opportunities during the conference. Our researchers are so grateful for the invaluable opportunity to have met and worked with so many families in person. And of course, an enormous shout out to the research teams for your time and dedication to the advancement of Batten research, and in particular, Dr. Jill Weimer and her team from Sanford Research who coordinated the mountain of logistics to make this happen.
Research Challenge videos: There’s still time to watch and vote!
Researchers worldwide have been asked to describe their most exciting Batten research in short, easy-to-understand presentations, with a maximum of 3 minutes and 3 slides (it’s not as easy as it sounds!). Please support our researchers, hear about the latest in the field, and VOTE via the yellow “Research Challenge” icon in the conference app. Thank you to all those who submitted an entry this year.
VOTING CLOSES ON SUNDAY, AUGUST 4.
Batten Disease Centers of Excellence and Affiliates Announced!
 During the Saturday evening Dinner Dance, we were thrilled to announce the five Clinical Centers of Excellence and four Affiliate Centers. The unveiling of the nine Centers, which represent the first in the reinvigorated Centers of Excellence Program, marks a significant step forward for Batten disease clinical care, support, and research in the U.S.
During the Saturday evening Dinner Dance, we were thrilled to announce the five Clinical Centers of Excellence and four Affiliate Centers. The unveiling of the nine Centers, which represent the first in the reinvigorated Centers of Excellence Program, marks a significant step forward for Batten disease clinical care, support, and research in the U.S.
Our heartiest congratulations to the Centers of Excellence: Children’s Hospital Colorado, Children’s Hospital of Orange County (CHOC), Kennedy Krieger Institute, Nationwide Children’s Hospital, and the University of Rochester Batten Center, and to the Affiliate Centers: C.S. Mott Children’s Hospital at the University of Michigan Medicine, NYU Langone Health, Rush University Medical Center, and UNC Hospitals.
BDSRA’s Center of Excellence Program aims to optimize patient outcomes, accelerate research, and improve the quality of life for individuals affected by Batten disease and their families by increasing access to the best possible clinical care and sub-specialty services through a national network of Centers. Families seeking clinical care for their affected loved ones can be confident that these recognized Centers are providing best-in-class, comprehensive care.
To learn more about the Program and our members click here.
Announcing the Batten Disease Global Research Initiative
 We are thrilled to unveil the brand new Batten Disease Global Research Initiative (GRI), a consortium of leading patient advocacy organizations worldwide, that share the common goal of advancing research for all forms of Batten disease. Together, our mission is to foster and collectively invest in the most promising research worldwide that seeks to address key research questions and areas of unmet need in Batten disease.
We are thrilled to unveil the brand new Batten Disease Global Research Initiative (GRI), a consortium of leading patient advocacy organizations worldwide, that share the common goal of advancing research for all forms of Batten disease. Together, our mission is to foster and collectively invest in the most promising research worldwide that seeks to address key research questions and areas of unmet need in Batten disease.
Representatives from all four consortium members were with us for the announcement, including the BDSRA Foundation (Amy Fenton Parker), BDSRA Australia (Dr. Ineka Whiteman), BDSRA Canada (President Lori Brown), and Batten Disease Family Association UK (BDFA, President Liz Brownutt).
Grants of up to USD $50,000 will be awarded for one year, with the potential of renewal based on outcomes in the first year. Funding will be provided by the Global Research Initiative, with financial contributions from the BDSRA Foundation, BDSRA Canada, and BDSRA Australia, with in-kind support from BDFA. In addition to this core funding, support is also being sought from other interested parties who may wish to partner on selected, subtype-specific projects, as our “GRI Funding Partners.” We are grateful to have already received interest from several potential Funding Partners including NCL Stiftung (Germany), Beyond Batten Disease Foundation, ForeBatten Foundation, and Noah’s Hope/Hope4Bridget Foundation.
If you are interested in becoming a GRI Funding Partner, please reach out anytime at research@bdsrafoundation.org.
And with that, we are pleased to share:
The Global Research Initiative inaugural Grant Round is NOW OPEN for Expressions of Interest.
To find out more about the Program and how to apply, please visit our site at battenresearch.org
Submissions CLOSE AUGUST 30.
Next month, we’ll announce winners from the NCL RESEARCH CHALLENGE video contest, and I’ll be sharing more about my recent visits to two Centers of Excellence and a tour of the laboratory of one of our best-known Batten researchers.
See you then and, as always, thank you for your support and dedication to our shared mission.
Warm regards,

CLINICAL PROGRAM UPDATES
Clinical Trial Tracker
Keep up-to-date with the latest clinical trial and natural history study news with our Clinical Studies Chart on BDSRA’s website. Check it out by clicking here.
Beyond Batten Disease Foundation/Theranexus – Batten-1 Program for CLN3 Disease
18 month data from Phase I/II trial of Batten-1
Together with Theranexus, the Beyond Batten Disease Foundation is pleased to share the latest press release reporting positive efficacy and safety data after 18 months of treatment for CLN3 patients in the Phase I/II Batten-1 clinical study. These results include reduced levels of a recognized neurodegeneration biomarker, consistent with the absence of marked motor symptom progression. Read more here.
BioMarin Pharmaceutical – BRINEURA® (cerliponase alfa) for CLN2 Disease
FDA Approves BRINEURA® for Children Under 3 Years with CLN2 Disease
On July 24, we were excited to share that the FDA has approved an expanded label for the enzyme replacement therapy Brineura. Originally approved in 2017 for use in symptomatic children aged 3 years and older, Brineura’s expanded indication now means Brineura is available for children of all ages with CLN2 disease, regardless of whether they are symptomatic or presymptomatic.
In the BioMarin press release, BDSRA’s Dr. Ineka Whiteman commented: “The opportunity to start Brineura treatment earlier, even before the onset of symptoms, provides newfound hope for the families impacted by this rapidly progressive disease. Importantly, this expanded indication provides further impetus for early diagnosis of CLN2 disease, as we continue advocating for inclusion of CLN2 disease on the RUSP (Recommended Uniform Screening Panel) for newborn screening.”
As many in our Batten community know, BDSRA Foundation Board Member Dr. Fernanda Leal–Pardinas, was formerly the Global Medical Affairs Lead for BioMarin’s CLN2 Disease program. Dr Leal-Pardinas shared some thoughts on these developments with the BDSRA Board of Directors this week, and has kindly permitted us to share it here:
This milestone is the culmination of 7 years of dedicated effort, which included conversations with regulators and additional research. The update profoundly highlights the critical need for early diagnosis and treatment of our children. The urgency of timely care cannot be overstated, as it is essential to prevent more damage. As we often emphasize: “time is brain.”
This expanded approval is crucial not only for the patients and their families but also for payers and healthcare providers. It underscores the importance of accessible treatment options and will likely shape future clinical trials and treatment protocols (potentially even for other types of Batten). Additionally, it may influence insurance coverage, making a significant impact on the lives of those impacted.
Moreover, this development is set to have international implications. Many countries look to the U.S. for guidance in healthcare practices, and this update may inspire similar actions worldwide, offering hope to families dealing with similar challenges.
Let us take a moment to recognize this progress as a sliver of hope. It reminds us of the importance of persistent advocacy and research, even when the path seems long and the outcomes uncertain.
Warmest regards,
Fern
The full press release from BioMarin can be read here.
RESEARCH OPPORTUNITIES
 New Grant Opportunity: The Global Research Initiative’s inaugural Grant Round is NOW OPEN for Expressions of Interest.
New Grant Opportunity: The Global Research Initiative’s inaugural Grant Round is NOW OPEN for Expressions of Interest.
To find out more about the Batten Disease Global Research Initiative’s brand-new Program and how to apply, please visit our site at battenresearch.org.
Submissions CLOSE AUGUST 30.
New research study: Decision-Making Surrounding the Use of Brineura in Patients with CLN2 Batten Disease 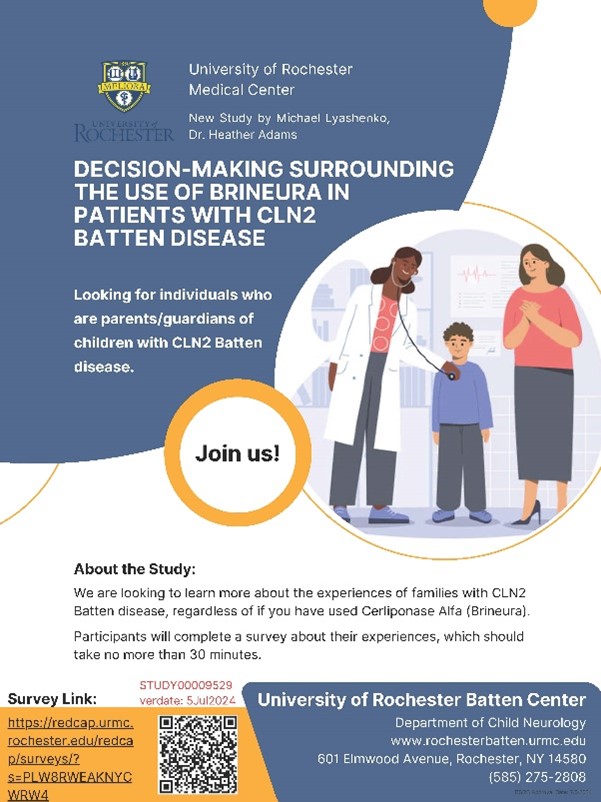
Principal Investigator: Michael Lyashenko
Co-Principal Investigator: Heather Adams, PhD
The University of Rochester Batten Center is conducting a study on decision-making about the use of Cerliponase Alfa (Brineura) in families of individuals with CLN2 Batten Disease. We are interested in hearing from all affected families, whether or not your child has ever received this treatment.
What is involved? Parents/caregivers of affected individuals who participate in the study will complete a survey about their child’s history of CLN2 Batten disease and Brineura use, as well as the reasons for the decisions made about its use.
Who may be eligible? Parents/caregivers of a child with confirmed genetic or enzyme-based diagnosis of CLN2 disease. If there is more than one affected child in the family, you may complete the survey for each affected child (if you wish to do so), or just one child.
No travel is required! All study activities will take place at your own home.
If you are interested in learning more about the study and participating in the survey, please click on this link or scan the QR code. Or, feel free to contact the study team at: Batten@URMC.Rochester.edu.
FAMILY REGISTER
Have you joined the Register yet?
The BDSRA Foundation Family Register is a vital tool that enables us to keep you informed of ongoing Batten disease research, including future clinical research and natural history opportunities.
The Register also enables BDSRA to understand more the prevalence of Batten disease, including the different subtypes and geographical locations. This helps us tailor our education and support activities according to the needs of our families. The Register is open to all current and bereaved families in the U.S. and internationally.
The information collected in this form is kept STRICTLY CONFIDENTIAL. Your involvement in this survey is entirely voluntary, and you may request to be removed from the list at any time. The form takes just a few minutes to complete and can be accessed by clicking here.
Thank you for participating in this important initiative!
PUBLICATION HIGHLIGHTS – July 2024
TRPML1 activation ameliorates lysosomal phenotypes in CLN3 deficient retinal pigment epithelial cells
Wünkhaus, D. et al. Sci Rep 14, 17469 (2024).
Mutations in the lysosomal membrane protein CLN3 cause Juvenile Neuronal Ceroid Lipofuscinosis (JNCL). Activation of the lysosomal ion channel TRPML1 has previously been shown to be beneficial in several neurodegenerative disease models. Here, we tested whether TRPML1 activation rescues disease-associated phenotypes in CLN3-deficient retinal pigment epithelial (ARPE-19 CLN3-KO) cells. ARPE-19 CLN3-KO cells accumulate LAMP1 positive organelles and show lysosomal storage of mitochondrial ATPase subunit C (SubC), globotriaosylceramide (Gb3), and glycerophosphodiesters (GPDs), whereas lysosomal bis(monoacylglycero)phosphate (BMP/LBPA) lipid levels were significantly decreased. Activation of TRPML1 reduced lysosomal storage of Gb3 and SubC but failed to restore BMP levels in CLN3-KO cells. TRPML1-mediated decrease of storage was TFEB-independent, and we identified TRPML1-mediated enhanced lysosomal exocytosis as a likely mechanism for clearing storage including GPDs. Therefore, ARPE-19 CLN3-KO cells represent a human cell model for CLN3 disease showing many of the described core lysosomal deficits, some of which can be improved using TRPML1 agonists.
Access the article here.
Reduction of neuroinflammation and seizures in a mouse model of CLN1 batten disease using the small molecule enzyme mimetic, N-Tert-butyl hydroxylamine
Fyke, Z. et al. Mol Genet Metab. 2024 Jul 15;143(1-2):108537.
ABSTRACT
Infantile neuronal ceroid lipofuscinosis (CLN1 Batten Disease) is a devastating pediatric lysosomal storage disease caused by pathogenic variants in the CLN1 gene, which encodes the depalmitoylation enzyme, palmitoyl-protein thioesterase 1 (PPT1). CLN1 patients present with visual deterioration, psychomotor dysfunction, and recurrent seizures until neurodegeneration results in death, typically before fifteen years of age. Histopathological features of CLN1 include aggregation of lysosomal autofluorescent storage material (AFSM), as well as profound gliosis. The current management of CLN1 is relegated to palliative care. Here, we examine the therapeutic potential of a small molecule PPT1 mimetic, N-tert-butyl hydroxylamine (NtBuHA), in a Cln1-/- mouse model. Treatment with NtBuHA reduced AFSM accumulation both in vitro and in vivo. Importantly, NtBuHA treatment in Cln1-/- mice reduced neuroinflammation, mitigated epileptic episodes, and normalized motor function. Live cell imaging of Cln1-/- primary cortical neurons treated with NtBuHA partially rescued aberrant synaptic calcium dynamics, suggesting a potential mechanism contributing to the therapeutic effects of NtBuHA in vivo. Taken together, our findings provide supporting evidence for NtBuHA as a potential treatment for CLN1 Batten Disease.
Access the article here.
Editorial: Neuronal ceroid lipofuscinosis: molecular genetics and epigenetics
Nicolaou, P. Front Genet. 2024 Jun 26:15:1430703.
No Abstract available.
Access the article here.
Neuronal ceroid lipofuscinosis in a Schapendoes dog is caused by a missense variant in CLN6
Bellamy, KKL, et al. Anim Genet. 2024 Aug;55(4):612-620
ABSTRACT
Neuronal ceroid lipofuscinosis (NCL) is a group of neurodegenerative disorders that occur in humans, dogs, and several other species. NCL is characterised clinically by progressive deterioration of cognitive and motor function, epileptic seizures, and visual impairment. Most forms present early in life and eventually lead to premature death. Typical pathological changes include neuronal accumulation of autofluorescent, periodic acid-Schiff- and Sudan black B-positive lipopigments, as well as marked loss of neurons in the central nervous system. Here, we describe a 19-month-old Schapendoes dog, where clinical signs were indicative of lysosomal storage disease, which was corroborated by pathological findings consistent with NCL. Whole genome sequencing of the affected dog and both parents, followed by variant calling and visual inspection of known NCL genes, identified a missense variant in CLN6 (c.386T>C). The variant is located in a highly conserved region of the gene and predicted to be harmful, which supports a causal relationship. The identification of this novel CLN6 variant enables pre-breeding DNA-testing to prevent future cases of NCL6 in the Schapendoes breed, and presents a potential natural model for NCL6 in humans.
Access the article here.
Neuronal Ceroid Lipofuscinosis in a Mixed-Breed Dog with a Splice Site Variant in CLN6
Mhlanga-Mutangadura, T. et al. Genes (Basel). 2024 May 23;15(6):661.
ABSTRACT
A 23-month-old neutered male dog of unknown ancestry presented with a history of progressive neurological signs that included anxiety, cognitive impairment, tremors, seizure activity, ataxia, and pronounced visual impairment. The clinical signs were accompanied by global brain atrophy. Due to progression in the severity of disease signs, the dog was euthanized at 26 months of age. An examination of the tissues collected at necropsy revealed dramatic intracellular accumulations of autofluorescent inclusions in the brain, retina, and cardiac muscle. The inclusions were immunopositive for subunit c of mitochondrial ATP synthase, and their ultrastructural appearances were similar to those of lysosomal storage bodies that accumulate in some neuronal ceroid lipofuscinosis (NCL) diseases. The dog also exhibited widespread neuroinflammation. Based on these findings, the dog was deemed likely to have suffered from a form of NCL. A whole genome sequence analysis of the proband’s DNA revealed a homozygous C to T substitution that altered the intron 3-exon 4 splice site of CLN6. Other mutations in CLN6 cause NCL diseases in humans and animals, including dogs. The CLN6 protein was undetectable with immunolabeling in the tissues of the proband. Based on the clinical history, fluorescence and electron-microscopy, immunohistochemistry, and molecular genetic findings, the disorder in this dog was classified as an NCL resulting from the absence of the CLN6 protein. Screening the dog’s genome for a panel of breed-specific polymorphisms indicated that its ancestry included numerous breeds, with no single breed predominating. This suggests that the CLN6 disease variant is likely to be present in other mixed-breed dogs and at least some ancestral breeds, although it is likely to be rare since other cases have not been reported to date.
Access the article here.